I looked down at the paper and read the words again: “George feels bad about himself, is frustrated with himself, is feeling discouraged, is not happy with his life, and is feeling incompetent.”
It wasn’t untrue, but to hear my own feelings so succinctly relayed back to me was a special kind of confronting. As is so often the case for me, another’s validation of my own interiority gave me breathing room — permission, really — to explore further, safely confirmed of the need to do so outside of my messy internal world. But all of that wasn’t exactly easy to hear, either.
The words staring back at me so starkly were the culmination of months of research and perseverance, and a lifetime of confusion of what exactly was going on in my head. It turns out the answer was, in a certain sense, simple:
I have ADHD.
I am five years old. I have cornered an older man at a grandparent’s birthday after having learned that he is a geologist. I have told him about my extensive rock collection at home, my frequent searches for new and interesting crystals, and I am now grilling him on exactly how volcanos form. This lasts for over an hour. I am in utter bliss.
What is ADHD?
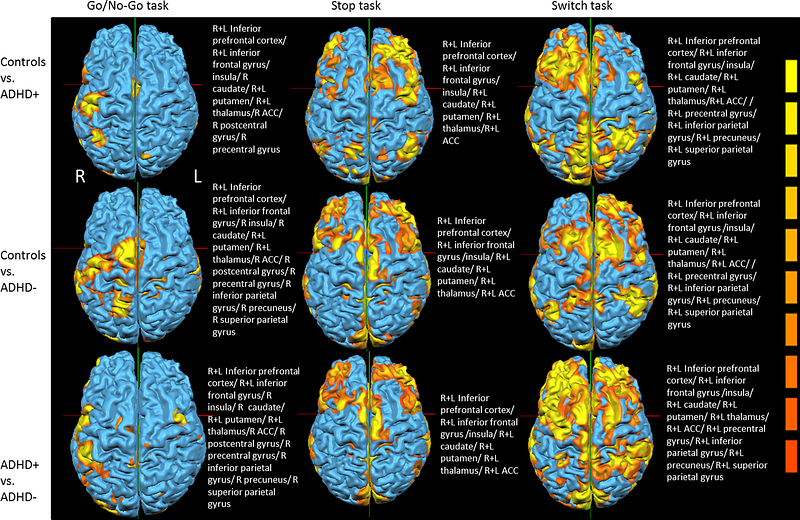
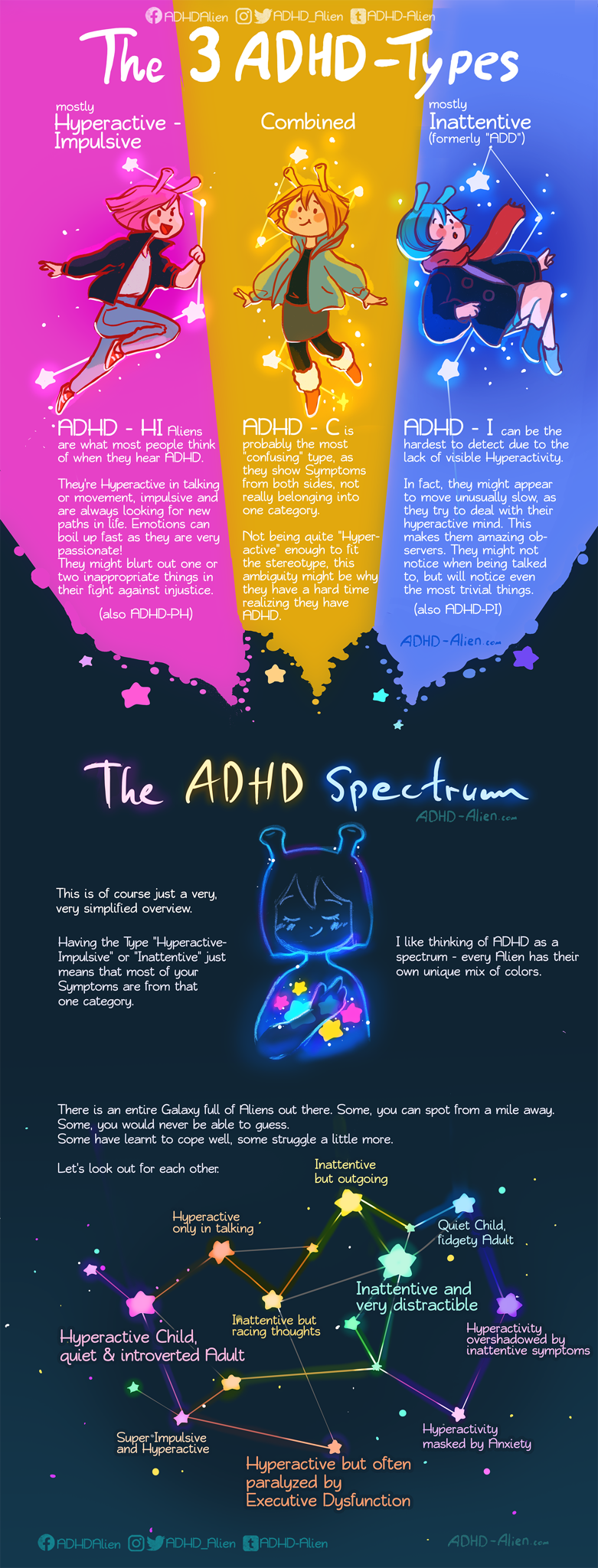
Attention Deficit Hyperactivity Disorder (ADHD) is a neurodevelopmental disorder characterized by inattention, excessive activity (mental and physical), impulsivity, and impaired decision making (called “executive dysfunction”). While there remains tremendous confusion about the disorder in the public discourse (even on what to call it!), the science is increasingly clear on the existence of the disorder, even as we struggle to understand its causes and permutations. What is clear, and in particular, from a 2021 “consensus statement” by leading doctors, researchers,and practitioners in the field, is that ADHD’s symptoms are definitively real and those with the disorder both requrie and deserve a variety of supports to enable them to live happy, healthy lives.
While the causes of ADHD remain elusive, as they do for many psychiatric conditions, the symptoms of the disorder have become more established and easier to navigate as both diagnosticians and patients. The experience of the disorder will vary immensely between patients, but the broad features are generally agreed to include:
Inattention – This includes behaviours or experiences like: extended and frequent daydreaming; high-level and frequent distractibility; difficulty finishing or organizing even simple tasks, but especially those with many steps or components; frequent losing of objects or forgetting of details; avoidance or extreme dislike of activities which require a high degree of focus or attention.
Hyperactivity and Impulsivity – This includes behaviours or experiences like: frequent fidgeting or squirming when required to be still; often leaving or moving when required to sit still; difficulty slowing down, both mentally and physically; excessive and fast talking; making impulsive decisions, such as related to buying things, gambling, substance use, sexual behaviour, and beyond.
It is important to note, as I’ll discuss later, that these behavioural features of ADHD are increasingly recognised as part of a spectrum, in similar ways to how Autism was reconceptualized into a single spectrum disorder in 2013. There, as of yet, has not been a formal reclassification of ADHD to this effect, but it is a lively area of research and convesation. But it is possible, perhaps even likely, that diagnosis and treatment of ADHD will move towards this more “dimensional” (i.e., something on a spectrum) approach over time and away from its current “categorical” (i.e., you have it or you don’t) diagnostic processes.
Something promising on this front is from the United States, called “Research Domain Criteria” (RDoC), which is an approach to studying mental illness was adopted by the National Institute of Health in 2010 and has some increasing sway in mental health research and practice. As NIH explains it, the RDoC “is a research framework for investigating mental disorders. It integrates many levels of information (from genomics and circuits to behavior and self-report) to explore basic dimensions of functioning that span the full range of human behavior from normal to abnormal.”
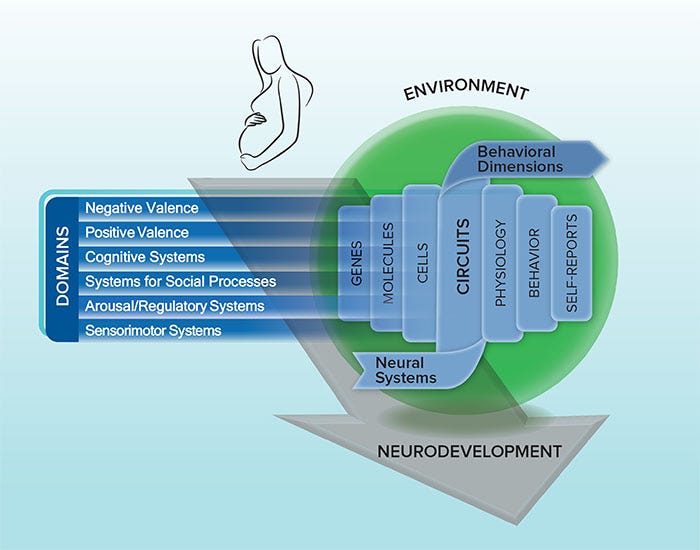
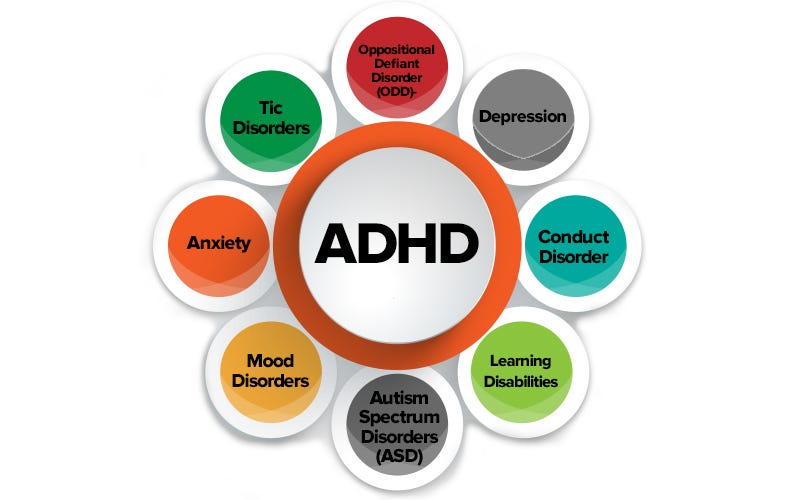
As someone now diagnosed with ADHD and seeing its interaction with other aspects of my life, such as anxiety and depression this makes sense on a personal level. But looking out more broadly in the world, and seeing the prevalance (“comorbidity”) of ADHD intermixed with other disorders, and the relationship of these disorders to brain structures, environment, genetics, and more, this seems analytically like a smart approach, too.
Are we sure ADHD is real?
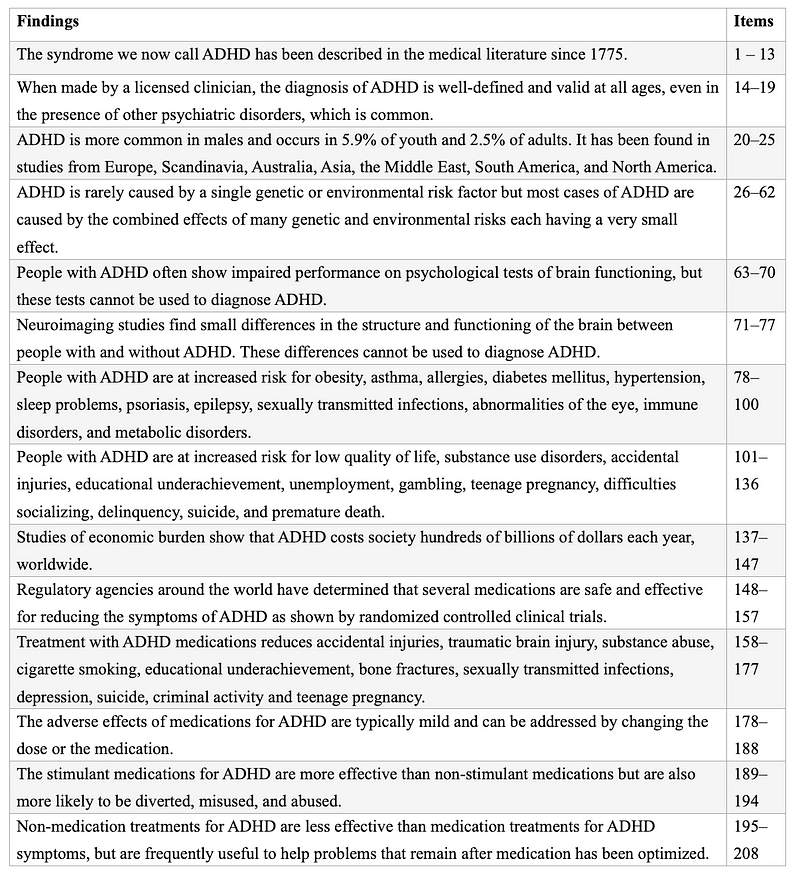
In 2002, and then again in 2021, a group of doctors, psychiatrists, and scientists published an “International Consensus Statement” which was emphatically clear that “ADHD is a real medical condition.” They wanted to once and for all make clear ADHD’s existence as a neurological condition based in the brain was undeniable, and while further research on causes and treatments was absolutely required, a binary debate about existence or not was no longer helpful .
While its existence has been confirmed and argued many times by researchers and clinicians, it is also true that some of ADHD’s manifestations, impacts, and treatments remain active areas of research, as they are for most conditions. In the 2021 statement, a prominent group of ADHD specialists were able to draw what they felt were 208 distinctive conclusions about the disorder, while still acknowledging where further research was needed.
The Consensus Statements were major milestones in what has now been a multi-decade debate on the reality and experience of ADHD. Much of this debate has been based on the comments of doctors, various psychological professionals, and writers (some of whom have not been well-rooted in the neurological literature of the disorder), who see ADHD and other conditions, such as Autism, as a result of the information age; unfair, culturally-specific expectations of behaviour; and even capitalism. In some of the simpler critiques, the disorder is simply a result of a society that (a) creates distraction constantly, and/or (b) requires a level of focus and attention that most humans are simply not able to sustain.
In any of these critiques of the medical nature of ADHD, there is often language that suggests doctors are needlessly overdiagnosing “kids being kids,” or that challenges associated with ADHD are not a disorder, but are simply behavourial problems and can be overcome with simple interventions like meditation, “digital minimalism” (which is good in and of itself, but not a fix for ADHD), and more rigorous planning. Important, as well, in much of this conversation is a belief by many that ADHD is harnessed by the pharmaceutical industry to sell drugs like Ritalin or Adderall, especially to young children.
And while over-diagnosis does appear to be a problem, any dialogue about the disorder must always recognise the lived experiences of people who have ADHD and who are asking for help, as well as the inherent diagnostic messiness of these kinds of disorders. Challenges of conceptual clarity, such as there are for some degenerative diseases, like ALS or MS, is not a reason to discard a field of work — but are in fact, as far as I am concerned, a reason to pursue even more rigorous and open-minded research and exploration.
Recent anthropology and historical research, however, is helping create some more solid foundations for this conversation. Perhaps one of the earliest instances of ADHD-like symptoms being researched and addressed was by Scottish physician Sir Alexander Crichton, in 1798. In a chapter of his second book On Attention and Diseases (as quoted in Lange et al, 2010), he defines inattention as “[w]hen any object of external sense, or of thought, occupies the mind in such a degree that a person does not receive a clear perception from any other one, he is said to attend to it.” A failure to “attend” to things, he theorised, “almost always arises from an unnatural or morbid sensibility of the nerves [emphasis added],” and “[this inattention] may be either born with a person, or it may be the effect of accidental diseases.”
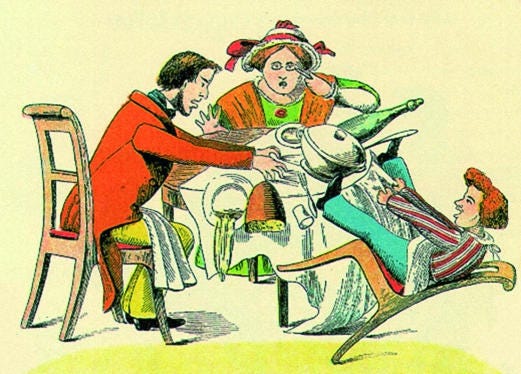
Another example is a 1845 children’s story written by a German doctor, Heinrich Hoffman, which speaks about a “Fidgety Phillip.” This tells a tale of a “naughty, restless child,” who breaks things and “screams with all his might” as he struggles to, as contemporary doctor’s might say, emotionally self-regulate.
As Klaus W. Lange et al detail, there are numerous other examples throughout history of similar observations, such Sir George Frederic Still’s work on children with a “defect of moral control” in the early 1900s, which, while not meaningfully characterizing ADHD in and of itself, was part of the arc of research asking questions about patterns of behaviour in the spirit of what we might today call “executive dysfunction.” Then there is the work German physicians Franz Kramer and Hans Pollnow “on a hyperkinetic disease of infancy,” which largely lays out diagnostic criteria similar in spirit to ADHD in the 1930s. Numerous other stories and research projects like this exist across history.
In short, ADHD is not an immediately modern phenomenon. While we cannot ignore the relative recency of studying the human brain and behaviours from what we might call “the medical model.” The “discovery” of ADHD and the rise of contemporary mental health are more or less inextricable, so, in the same way, it is important to see ADHD, like depression, borderline personality disorder (BPD), post-traumatic stress disorder (PTSD), autism spectrum disorder (ASD), and many other mental conditions, as part of the growth of medical and psychological research in the past hundred and fifty years. In this, ADHD has evolved the same way that cancer research has, moving from simple theories of it being contagious, to a complex, nuanced field of study and practice.
Based on my personal readings and learnings over the course of writing this article, I have no doubt that both the diagnostic processes and the treatments associated with ADHD (and related conditions) will change and evolve over time. Shifts from a dimensional to a categorical approach may even one day change or reframe the disorder quite dramatically. I have no issue with this insofar as the needs of those of us who need help continue to be recognised and addressed by researchers, practitioners, and the public at large. Indeed, a broader reframing of the disorder may even broaden our societal horizons of what it means to have a healthy brain — something that seems sadly needed in a world still pathologically terrified of the “mentally ill.”
I am sixteen years old. I am trying to leave to meet my friends at the mall; I cannot find my keys. Not only can I not find them, they no longer exist. This is the third time this month that I have lost them, and a spare set my parents have given me. I feel ashamed and frustrated at my carelessness. In addition to my keys, last month I also lost my wallet; forgot my login to my Facebook account, and didn’t submit an assignment on time because I mixed up the days. My parents are angry with me, and a deep fear wells up inside of me that my friends’ and family’s patience with me is at its end. I am ashamed.
What causes ADHD?
The direct and exact causes of ADHD are unknown. Isolating a direct cause, such as a mutation in a single, specific gene for a complex disorder like ADHD is inherently challenging, and likely impossible. This is because of the multiple genetic and environmental factors that are behind it. This is similarly true for Autism Spectrum Disorder (ASD) and other, related conditions. As a significant review of medical practitioners working on ADHD in 2012 said succinctly:
“No single risk factor explains ADHD. Both inherited and non-inherited factors contribute and their effects are interdependent. ADHD is familial and heritable.”
ADHD research over the decades has laid out elements of what causes the disorder, which include both genetic and environmental causes. Some of these include:
- Having a biological relative with ADHD
- A significant structural variation in a person’s genes, such as “large, rare copy number variants” [in your DNA];
- Some small effect size candidate gene variants,
- Extreme early adversity,
- Pre and postnatal exposure to lead; and
- Low birth weight/prematurity.
While each and all of these have been consistently found as risk factors for ADHD, none has yet been proven to cause the disorder all on its own. Additionally, outside of the general cases where ADHD has multiple drivers, there are rare instances “where ADHD-like symptoms can be caused by extreme deprivation early in life, a single genetic abnormality, or traumatic brain injury early in life.” For me, the exact combination is unclear and, on some level, irrelevant — most saliently, I suspect some manifestation of ADHD is likely throughout my family, and coincides with other (epi)genetic factors.
How does ADHD relate to broader movements around mental health?
The struggle for recognition, treatment, and de-stigmatization around ADHD does not exist in a vacuum. In fact, it is part of a much larger struggle for a number of movements related to various mental disorders to gain respect and support.
Many of these are categorized broadly under the idea of “neurodiversity.” Neurodiversity, or neurodivergence, is a concept that often is used to encompass ADHD. It is a complex and sometimes controversial term that fundamentally refers to the idea that people with ADHD and similar conditions have differences (“divergence”) in their brains that are part of a natural variation amongst humans. Part of the appeal of this neurodivercene framing is that it also can make clearer many of the the subtle, and sometimes large, differences between people who have the same diagnosis, but radically different experiences of the condition.
Furthermore, many conditions (such as ADHD and autism) often exist together (i.e., are “comorbid”) and so separating out symptoms and their interactions can become extremely complex, depending on the person in question, and make diagnosis and recognition difficult.
There is a significant body of literature on neurodivergence, much of which is sociological or anthropological in nature. Often, it makes the case that the medical language and framing, and particularly the emphasis of some on medication and management of symptoms, can generate shame or misunderstanding around what ADHD is and those who have it. Controversy has arisen, though, around the subtleties of these points: some with ADHD, and in other disability communities, feel that “divergence” trivializes the feelings of those who have a disorder that causes genuine pain and discomfort, and material impacts (e.g., people with ADHD face cost burdens and lost income worth billions every year in the US alone).
On a personal level, I have sympathies to both views, and genuinely see the neurodivergence movement as offering helpful language and criticisms of the medical model. At the same time, some of the broadness of “ND” conversations worries me in that it may trivialize those who struggle more to function in socially acceptable ways. As a seemingly “high functioning” neurodivergent person, I worry that my experience, and others like me, may overshadow those who suffer more acutely than I do — whatever their brain may be experiencing. I feel responsive to the types of criticisms that are often expressed against “white feminism,” wherein those who experience less acute forms of marginalization sometimes become the face of a de-stigmatizing movement with widely different experiences across its members. While I hope to be able to raise awareness in my own way, I recognise that listening to and, where appropriate, advocating for those with needs greater than my own is the best way to achieve the world we both need.
In the broader social world, the dividing lines between those who think neurodivergence adds something to conversations around ADHD and other disorders, and those who do not, can be quite stark. However, as the conversations broaden and more people participate, the ADHD community on Reddit (one of the largest in the world), recently began a dialogue on their frustrations and concerns with the neurodiversity movement, and how it treats this disorder. I like the way this dialogue played out and, while hardly perfect, feels meaningful to me in that it is between people who all share a common experience and is working to establish terms for them — for us — to use as part of the struggle for equality.
In a thread on r/ADHD, moderators and top commentators on the subreddit outlined their frustrations and their sympathies between a more medical view of the disorder, and the more sociological one. Ultimately, they disagree with many of the actors and behaviours of those in the online neurodiversity communities they’ve encountered. I can’t and won’t speak to that, but in reading their, and several other, summaries, their engagement with the topic felt fair overall. And while it lacks the formality of a medical journal or large publication, its casualness and honesty were deeply refreshing and spoke at a community level to many things I think are important.
The thread, written by one of the moderators of the sub-reddit, u/bipb0p outlined the areas of agreement and disagreement between a more medical view of ADHD and the neurodiverse view as follows:
What beliefs do [those who use more of a “medical model” of ADHD and the Neurodiversity movement] have in common?
- We acknowledge that mental health disorders are highly stigmatised and misunderstood.
- We agree that people with mental disorders have a right to equitable access and participation in society.
- We agree society disadvantages those with mental health disorders and we should accommodate these people as best we can.
- We believe that both the medical and social models of disability warrant consideration.
- We want greater patient autonomy in treatment.
- We believe people with ADHD are capable of leading happy, fulfilling lives.
- We acknowledge that psychology and psychiatry are not perfect. We acknowledge its historical harms, such as: (1) failure to provide equal access to treatment; (2) failure to ensure proper representation in academia and research; (3) and causing harm at higher rates to marginalised groups such as people of colour or LGBTQIA+ people.
Where do we disagree?
- We disagree with the common assertion that mental health disorders are just “differences in cognition.” These conditions come with very real innate harms.
- We feel the social model creates a distinction between impairments and disability, which causes people to overlook the potentially life-threatening impact of impairments. For many people, our innate impairments can be just as disabling as the oppression of society, if not more so.
- Parts of the movement appear to be distancing themselves from the term “disability” as if it is somehow an admission of weakness. We feel that rejecting any association with disability is ableist and dismisses those of us who require higher levels of care.
- We firmly believe there is a very real risk in framing mental health disorders as “gifts”, “beneficial” or “positive states.” Such claims would lead those in power to believe that we don’t need/deserve medication or accommodations.
- The medical model of disability is frequently rejected by the movement and we cannot accept this. We deem it a necessary foundation that enables the treatment of ADHD and many other mental health disorders with medicine and other medical interventions. We believe that both the medical and social models of disability are valuable and necessary tools for achieving our fundamental goal: improving the lives of people with ADHD.
There’s tremendous nuance that anyone on either side of this argument could make. Perhaps the distinctions which I think are gently and reasonably drawn here, could be shifted or expanded further. But the commonalities are powerful. And the suggested differences feel like the areas I want to explore most.
In the end, I feel comfortable to use the term neurodivergence for myself, and want to carefully ally myself with the movement’s intentions insofar as they respect the medical model, centre the needs of the disabled, and recognise the often deep harms of these differences while still creating space for celebrating excellence and accomplishments of disabled people.
I am twenty-two years old. I have barely slept this week, but I have completed all of my school assignments, hosted my course-union meeting, attended every party I was invited to, and helped run an international conference. I am working on a personal writing project in the wee hours of the evening each night. Bags have formed under my eyes, but my smile never falters. I am succcessful, fulfilled; I am on a razor’s edge.

What has this meant for me?
I have lived with, and often suffered from, anxiety and depression all of my adult life. It has taken time to feel comfortable to talk about it more openly, but I have been in various types of counselling and therapy since I was nine-teen to work on and live more in balance with these parts of myself. When I finally did get my ADHD diagnosis, I looked back somewhat bemusedly at all of the therapeutic and educational experiences I had had and wondered why no one had ever said anything. When I told loved ones and colleagues of my diagnosis, the most common response was generally “oh, that makes sense.”
So, where did so many people, myself included, miss the signs?
There’s a phrase in a lot of the literature around mental health that makes me very uncomfortable, but which is often applied in situations like mine: high-functioning.

High-functioning is a very loaded phrase. It’s been in the psychological literature for a long time and has a number of interpretations. It rests upon an even deeper and more contested series of ideas and observations about what it means to ‘function’ at all. From a baseline understanding of what a neurotypical (i.e., a statistically average) human brain ‘should’ act like, researchers and practitioners have layered in observations and theories about the deficits in cognititive ability (and otherwise) that ADHD, or any other conditions, cause. From a series of assumptions about an expected average social performance, a varyingly vast or slapdash heuristic analysis can be undertaken: measuring, or observing, the outcomes of the disabled against some generic social average. The difference (higher or lower) between an statistically average person, and a disabled/divergent person, represents the degree to which they may be “high- or low-functioning.”
This kind of calculus, however, is impossible to standardize concretely, particularly for disabilities as varied as ADHD and many related forms of neurodivergence.
As one example, Teresa Torralva et al implicitly define it rather narrowly in a 2012 abstract as a person with “a convincing history of real-life executive deficits perform[ing] entirely within normal limits or with minimally impaired performance in classical executive tests.”
In contrast, Klaus-Peter Lesch offers something simple, but profoundly broad:
An individual who fully meets the criteria for ADHD, but still is able to function relatively well, is described as having high-functioning (HF)-ADHD, with some ADHD expressions being severe and others located more towards the mild end of the diagnostic spectrum. [emphasis added]
I think Lesch’s definition hits a little more closely at what makes me uncomfortable about this whole idea, though later in the article he’s quite kind and sympathetic to the full experience of those who are “high functioning.” However, his use of “relatively” and “well,” pedantic as it may sound, should focus our attention: relative to whom, and well on what bases? Toralva and many others opt for a more circumscribed definition around standardized tests — which, as we can all imagine, have many flwas — but in doing so, they remove some of the epistemic trip-wires that emerge when we compare humans on such a broad basis.
A contradiction emerges from these two frames for “high-functioning.” It is where I share sympathies with the social model of disability and Mad Studies, in that they and I agree that the values inherent in the idea of “high-functioning” are specific to the society that we live in now and all of its injustices.
For people like myself, with advanced degrees, middle-class income, strong social connections, and so on, it coud be fairly said that I am high-functioning not only in relation to some of my ADHD peers, but across society at large. Stack that on top of the other privileges I have as a white, cis man in a wealthy country, and it’s easy to see why some people like me really like to see ADHD as a “superpower” — and, indeed, perhaps this is why my diagnosis took so long.
From an external perspective, my societally acceptable success means I am “high functioning.” Indeed, unless there are visible problems, there’s probably no need to worry — or, perhaps, even to diagnose. This is a common experience I have now seen across people with ADHD who openly discuss their diagnoses online. This burgeoning culture of visibly ADHD people in public life, while it has many limitations and downsides, has been on balance an indescribable gift and comfort to me.
I have seen so many people now talk about decades of self-loathing, anxiety, social isolation, and guilt while performing “relatively well” (sorry, Lesch) in societal terms.
A common occurence for those of us of this type, which generates phenomenal guilt, shame, and stress, seems to be a two-fold incongruity:
Firstly, many of us in this high-functioning camp are good at a variety of creative, socially prestigious tasks. My brain loves a knotty, complex problem. In fact, it’s really the only kind it likes. The more straight-forward a problem (especially if it involves no bodily movement or is otherwise un-stimulating), the less likely I am to engage. Update my ID so I can travel? Psh. No thanks. Solve your multi-party, resource-constrained wicked problem? Let’s go! (Did I mention I work on climate change?) Being willing and able to take on these kinds of tasks is, understandably, a strong source of social status.
Secondly, many of us still struggle with the most basic aspects of functioning, because of how profoundly uninteresting they can be. And from that, being the person who has lost their keys for the seventh time that month does not net you any social gravitas. Furthermore, it contrasts so visibly with your performance elsewhere, that people’s perception of you can whiplash between hypercompetence and near-buffoonery. The phrase “absent-minded professor” has been used on me more times than I’d like to count. And while it can be funny at first for people that are just meeting you, I’ve had to work incredibly hard to minimize these tendencies with loved ones, and to beg for their patience and forgiveness for the things I struggle with most, especially navigating complex processes, remembering important (but uninteresting) details, and making certain kinds of decisions.
Perhaps even more insidiously, the distance between these two experiences is most magnified in my own consciousness. Attacking a complex problem brings me such joy and I believe is something I genuinely excel at. And yet, since being diagonsed with ADHD months ago I have lost track of the number of times I have tried and failed to book a doctor’s appointment to continue treatment. Sometimes it’s hard for me to make sense of myself, let alone for others to understand why I can do some things so well, and others so poorly.
It’s difficult to to put into words the pain that this incongruity causes me internally. I have been profoundly, existentially unkind to myself over many years because of these feelings. It has led me, in sometimes curious ways, to adopt patterns of behaviour I believe no longer serve me. Taking on innumerable projects, causes, and ideas, all with the intention to scratch that dopamine-hungry itch is a common response to my boredom or need for novelty. Dangerously, it also has allowed me to construct a lifestyle where urgency and pressure are omnipresent. I am proud to have accomplished all that I have in my short time on this earth, but it has come at an immense cost. The stress of potential failure keeps me motivated, but, as I enter my thirties, it has also left me profoundly drained and, though it is difficult to admit to, burnt-out.
It’s a strange thing. The internal forces that have helped me accomplish — and desire — much of the external success I have achieved, have also hampered and hobbled me in perhasps some of the most intimate ways that I can imagine.
I think that’s what in therapy they call “a breakthrough.”

I am thirty-years old. I notice a restlessness in my muscles. I cannot concentrate and my internal monologue is internally harsh in turning my attention back to the task at hand. I notice this and close my computer. I stand up and take stock of how each part of my body feels. I go for a walk and give myself permission not to feel guilty about needing one. I am trying.
What now?
Since receiving my diagnosis, I’ve been on a winding pathway to understanding and learning more about myself. To say that this diagnosis has changed me in some dramatic way would not fully be true. I remain the complex, confusing human I have always been. But it has exposed and called into question most of the day-to-day thoughts, feelings, and behaviours that make up my life.
Interestingly, I have heard some people experience this questioning as something profoundly challenging and exhausting. But for myself, this invitation to examine the quotidion and the seemingly benign parts of my life has been often-relieving, and sometimes exhilarating.
Numerous areas where I have been challenged throughout my life now feel like reasonable areas to question received wisdom of how I “ought” to do things. The one-million small shoulds, oughts, and musts that I have berrated, villainized, and lambasted myself over now feel ready to be examined more dispassionately. After almost two decades of seeing myself through a lens of moral failure, that kind of self-appraisal suddenly feels unacceptable. Having external validation of a longstanding feeling of something inexplicable and indescribable has created profound new space.
To some this may sound overrought. But the unvarnished truth is that there have been parts of myself that I have come to hate, particularly as I have entered into my late twenties and now thirties. I had come to see the things I struggled with as moral failings that not only illustrated laziness or poor judgement, but a sign of unlovability.
Thank god for Mitski — the perfect soundtrack to any voyage of self-discovery.
To let go of some of those feelings — or at least feel like I can push back against them — has been restorative in profound ways. I feel more connected; more worthy; more human.
As an outcome of this process, an increased sense of connection has perhaps been one of the most unexpected and appreciated upsides. A common thread across many the people I love these days has been a sense of internal curiosity. Maybe it’s the pandemic, maybe it’s that many of us are headed into our thirties, but everyone I know seems to be asking these questions of themselves these days. Thank goodness! These parallel processes of discovery have enabled incredibly rich conversations about both shared and differing experiences of neurodivergence — ADHD, autism, processing difficulties, and many others — and, crucially, of trauma.
It is not surprising that the most incredible feeling, post-diagnosis, has been moments of recognition and acceptance. All those moments of childhood and adolesence (and some in adulthood, too) of simply not understanding why I was wrong, why the thing I wanted to do, or couldn’t do, simply could not happen, suddenly feel contextualized. Sadly, there are many deep — and subtle — wounds that will take time to heal. But sharing and talking with friends about these issues for the first time has already been immensely healing.
Both the exciting and the frighening thing of where I am now, is that there are no next steps. There’s no ten-point plan. No guranteed, sure-fire way to address some of these challenges. The anxious people-pleaser in me was horrified (and then later pleased) to learn that some of my challenges really will never disappear. I’ll never be good at some things. (That still stings a little).
But that’s okay. I’ll be okay.
If I keep working at this, I think, I might just be better than okay. I might even be happy.
Some Thanks
Perhaps in classic ADHD fashion, I forgot something after I wrote this: prior to starting to write this article, I was blessed to be surrounded by some wise and generous people who gave their time to me to help make sense of this diagnosis. The help and, more importantly, the comradeship of James Glave, Grace Nosek, Ingrid Valou, and Kelsey Taylor was invaluable as I wrote this and I’m deeply grateful to them, and many others, for their ongoing support.

Sign up for George Patrick Richard Benson
Strategist, writer, and researcher.
No spam. Unsubscribe anytime.

